Main points
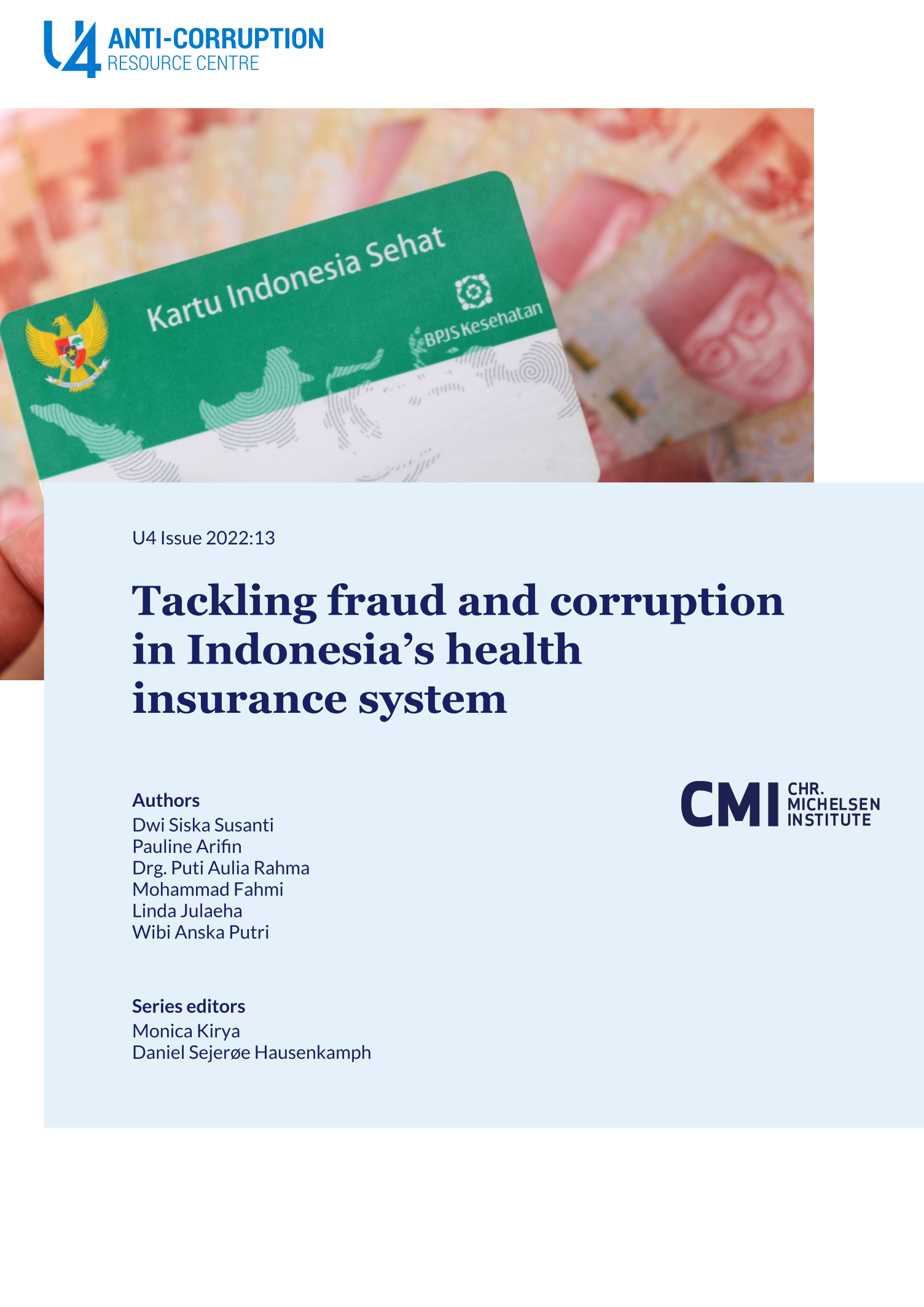
- Since its creation in 2014, Indonesia's National Health Insurance programme (JKN) has had a positive impact on access to health care, even though it is underfunded. Addressing corruption is crucial in order to safeguard the funds available.
- Fraud in national health insurance schemes can include billing for services not rendered, unnecessary medical tests and treatments, kickbacks, third-party fraud, and bribery, among others.
- Fraud and corruption in the JKN programme cause significant financial losses and decrease health care quality and access.
- During the Covid-19 pandemic, the risk of fraud and corruption increased due to uncertainty and disruptions arising from the emergency. These allowed different actors to take advantage of the situation for private gain.
- Despite some progress in addressing fraud and corruption, efforts to strengthen measures at the central and subnational levels remain inadequate and have not been implemented optimally. This is due in part to lack of clarity on responsibilities and an absence of clear guidelines on fraud risk management.
- Future interventions should be based on a thorough fraud risk assessment as the basis for targeted and feasible measures to mitigate fraud and corruption risk.